5 Myths About Schizophrenia

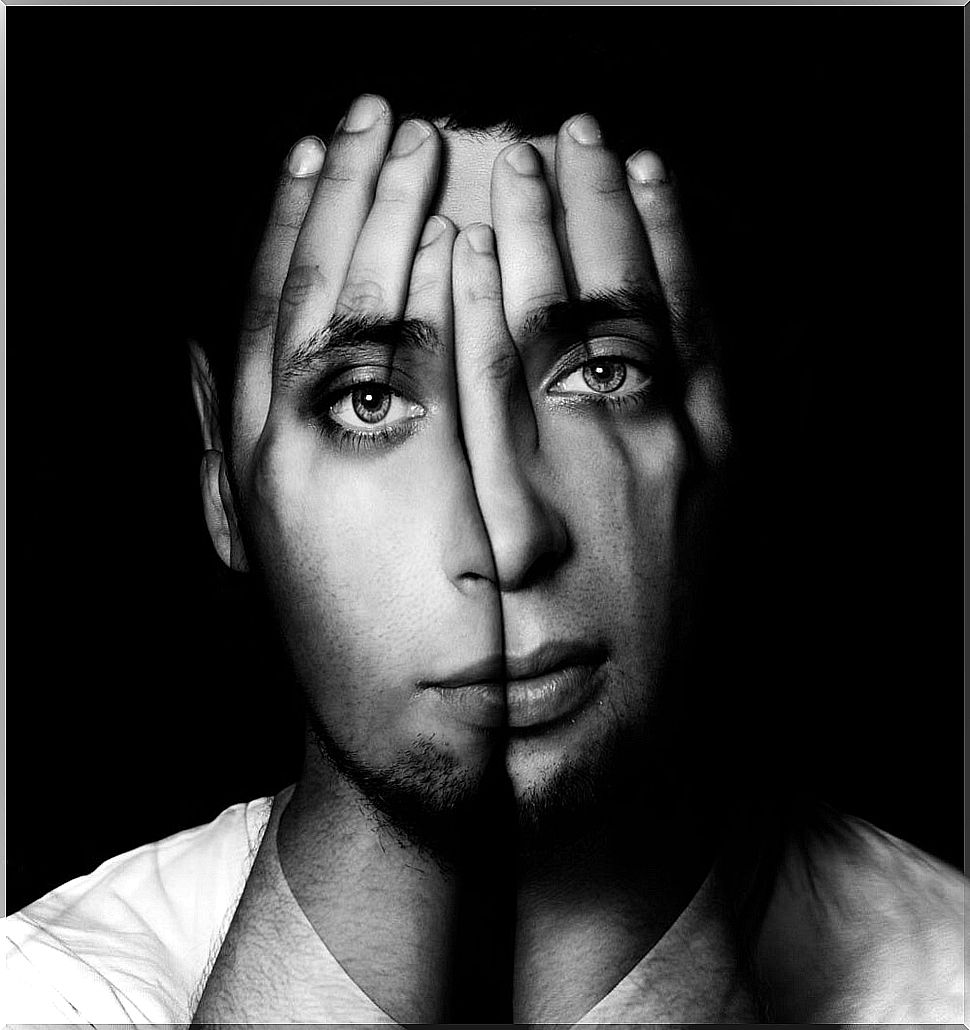
Schizophrenia is one of the most complex mental disorders, it is also one of the most misunderstood and with which mental health professionals least agree. Thus, people diagnosed with schizophrenia often suffer stigmatization and discrimination from their environment.
Being diagnosed with schizophrenia is a great personal burden on an emotional level. Since these people are labeled based on a series of symptoms, related to a frequent disconnection with reality. Something that in our society is associated with madness.
There are many misconceptions about how people are diagnosed with schizophrenia. Beliefs that have been fueled by ignorance, ignorance, and fear of the unknown. In these 5 myths we collect some of the most widespread misconceptions about schizophrenia.
1. People diagnosed with schizophrenia are dangerous and unpredictable
This is one of the most widespread myths, since the media themselves often associate this disorder with violent events. However, they are not more violent and aggressive than someone else in the general population can be. These people, when they suffer from a psychotic break that leads to hallucinations and delusions, are often afraid, tend to be isolated and more vulnerable, being victims of violence above all.

Aggressions occur due to causes associated with addictions, drug use, unfavorable social circumstances and the abandonment of medication. In the social stigmatization of schizophrenia, its symptoms are related to unpredictable behaviors that can become violent. When in fact they are specific events by a minority, for reasons other than schizophrenia itself.
2. Intelligence in people with schizophrenia is affected
They may experience difficulties in concentration, attention, memory, organizing their thoughts, and processing. Many of these symptoms are side effects of medication: antipsychotics, anxiolytics, mood stabilizers, and even antidepressants.
Cognitive symptoms associated with schizophrenia are presented under: disorganized thinking, lack of initiative and planning, as well as difficulties in setting goals. These symptoms are related to executive functions, similar to those suffered by people who suffer from damage to the prefrontal structure of the brain.
According to David Shakow: “The schizophrenic patient has conserved sensorimotor abilities, as well as several intellectual abilities, but these intact functions coexist with a fragmentation, stereotyping and disorganization of the types of behavior that require verbal or symbolic representation”.
In schizophrenia, intelligence is well preserved, however, its lack of intelligence tends to be confused with other functions that are affected. Although with difficulties, these people can harbor great capacities in creative, logical-mathematical, linguistic-verbal processes, and other areas of intelligence, acquiring a good development in these competences.
3. The main cause of schizophrenia is genetic
Genetics play a very important role in explaining schizophrenia, however, it needs many other causes for it to appear and develop. After many investigations it has been possible to verify that it does not have a single cause that is responsible in its entirety.
Schizophrenia has its appearance, explanation and evolution in multiple implicated causes. The investigations declare possible causes at the brain level, an implication in the genes and ultimately a biological predisposition that interacts with social and psychological factors.
All these factors play an important role, so associating schizophrenia only with the genetic factor is not the most convenient, something that on the other hand is usually a common mistake. The right thing to do is to assume the interaction that exists between genetic predisposition and the environment.
4. Schizophrenia can only be treated with drugs
Antipsychotics or neuroleptics are the main drugs that most psychiatrists recommend when making the diagnosis of schizophrenia. However, the drugs by themselves are not a guarantee of anything, since they have side effects that reduce the quality of life of these people.
Although in cognitive symptoms and “negative symptoms”, related to affective flattening, social isolation, lack of interest and initiative to undertake activities; It is essential that there is psychological support, so that the diagnosed person can have a certain quality of life.
When both therapies are combined, the pharmacological with the psychological, the evolution of the person diagnosed with schizophrenia is much more favorable. In the words of Carl Gustav Jung in his book “The content of psychosis”: “the path to the psychiatry of the future, which should better understand the essence of the matter, is clearly marked: it can only be the path of psychology. That is why in our clinic in Zurich we have dedicated ourselves to the psychological investigation of mental illness ”.
5. People with schizophrenia cannot lead normal, productive lives
Thanks to research in the pharmacological field and its integration with psychological treatments, it is being achieved that the symptoms of schizophrenia have less and less impact on daily life. Thus, many of those with schizophrenia can already lead productive and satisfying lives, despite the difficulties they encounter.
In addition, there are more and more cases in which the symptoms of schizophrenia recede with age, tending to stabilize. Therefore, the remission of schizophrenia is clinically feasible and real, as has been proven (Ciudad, Antonio, et al 2011).
Consulted bibliography
- Jung, CG (1990). The content of psychoses: psychogenesis of mental illnesses, 2.
- Laing, RD, & Schatzman, M. (1978). Schizophrenia and social pressure. I. Vericat (Ed.). Tusquets.
- Ciudad, A., Bobes, J., Álvarez, E., San, L., Novick, D., & Gilaberte, I. (2011). Relevant clinical outcomes in schizophrenia: remission and recovery. Revista de Psiquiatría y Salud Mental, 4 (1), 53-65.
- Esbec, E., & Echeburúa, E. (2016). Violence and schizophrenia: a clinical-forensic analysis. Yearbook of Legal Psychology.